Proper mammographic positioning is essential to the detection and diagnosis of breast cancer. Without properly positioned and exposed images, the radiologist cannot clearly find the presence of abnormalities which would possibly require a biopsy. Skilled, dedicated mammographers must recognize the importance of their role and must always pay close attention to detail so they can produce high-quality, mammograms on behalf of both the patient and the radiologist. This requires ongoing education and a thorough understanding of normal breast anatomy.
A mammography technologist is responsible for positioning the breast in accordance with the 1999 American College of Radiology (ACR) positioning guide. According to Deborah Thames, lead technologist at MD Anderson Cancer Center in Houston, Texas and MTMI Instructor, an in-depth knowledge of breast anatomy and physiology can help improve technologists’ ability to perform quality mammograms.
When should screening mammography begin?
Women at average risk of breast cancer should have a mammogram performed annually, starting at age 40. According to the ACR a risk assessment should be done by age 25 to determine if a woman is at a high risk for breast cancer. Women with higher-than-average risk should begin regular mammography as soon as age 30 but never sooner than age 25. Though rare, breast cancer can develop in a young woman, however, the younger you are, the more sensitive the breast tissue is to radiation. Other screening tools such as an MRI or Breast Ultrasound can be used in conjunction with mammography or instead of mammography depending on the age of the patient and their individual risk.
What are the different mammographic exams?
Screening mammograms are performed on asymptomatic women that have no breast problems or new breast concerns and consists of 4 images, 2 on each breast. The breast consists of layers of soft tissue, and can vary in size, shape and thickness from patient to patient. Standard screening views put in laymen’s terms are one view of the breast positioned so it can be compressed from top to bottom and another view of the breast positioned so that the breast is compressed from side to side. These standard views are performed at every mammogram exam.
When the two standard views fail to capture 100 percent of the breast tissue, supplemental views may be utilized. A patient’s body shape may inhibit the technologist’s ability to capture enough breast tissue so the technologist can make the judgment on adding supplemental views. Other factors may also come into play such as mental or physical disabilities and supplemental views may be easier on the patient verses standard imaging.
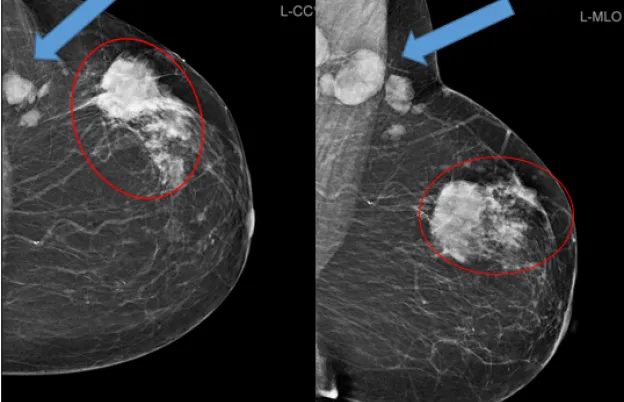
A diagnostic mammogram will include the standard views but often requires the use of dedicated additional mammographic views or an ultrasound to provide the radiologist with more detailed information. For patients with new breast concerns or patients that had a recent screening mammogram that showed an abnormality, a diagnostic mammogram will be performed. These additional views can help a radiologist determine whether an abnormal appearance is suspicious enough to warrant a breast biopsy.
How is mammography positioning different than other body parts?
Most radiographic positioning involves bone structures, which are relatively standard anatomically from patient to patient. Technologists position patients to show frontal, lateral, and oblique angles of bones to reveal fractures and/or diseases. Regardless of the patient's body habitus, radiology technologists position most patients the same in every case, meaning there is a high degree of standardization.
On the other hand, mammography positioning involves soft tissue structures. Each patient’s breasts are different sizes and shapes. Mammography technologists need to become well acquainted with these variations and be able to skillfully position the breast to capture high-quality images for the radiologist. Not only does the mammographer have to be able to accommodate these differences adequately, but they must also account for the patient’s body habitus, which could prohibit good standard imaging. The ACR has recommendations for breast positioning for the “non-average” patient to assist in capturing as much breast tissue as possible. Still, given the variations in breast size and shape and the potential limitations in patient mobility, mammographers must develop unique skills in positioning to acquire the images necessary to capture the whole breast in the fewest number of views possible.
ACR Mammography Positioning Guidelines
The American College of Radiology (ACR) is an accreditation body that provides feedback on the quality of clinical images performed on mammogram units. The feedback gives information on 8 attributes of the images that are important for the quality of the mammogram. The staff is also checked for initial training qualifications, continuing education and continuing experience requirements. The quality of the mammography unit is graded with a phantom image acquired on that individual unit. All must be in accordance with the Mammography Quality Standards Act (MQSA).
EQUIP
Most of the accreditation deficiencies in mammography are the result of poor positioning and compression. In an effort to improve mammography positioning, the FDA implemented the Enhancing Quality Using the Inspection Program (EQUIP) in 2016. In order to ensure that a facility is continuing to comply with the imaging standards set forth by their accreditation body, facilities should randomly audit the positioning work that they do. This is done in part by ensuring there is an established workflow for how to handle the need for corrective action with regard to image quality and secondly by randomly auditing the positioning quality of all active technologists. Since the interpreting radiologist is the only person who can determine if corrective action is needed, each active interpreting radiologist must be randomly audited as well to ensure they are not accepting images of poor quality. Lastly, all facilities must ensure that their mammography lead interpreting physician (LIP) is overseeing their QC/QA program. This means the LIP is reviewing quality control records, ensuring regular equipment maintenance is performed, and corrective action is taken when necessary.
FDA-approved accreditation bodies, such as ACR, conduct a random image validation check (IVC) on 300 facilities each year to check on the quality of the mammographic images performed at those facilities and determine whether a facility is upholding required quality standards. A strong EQUIP program will ensure a facility will be able to pass an image validation check if/when their facility is audited.
Standard Views
Craniocaudal (CC) View (in laymen’s terms the top to bottom view)
The craniocaudal (CC) view is typically performed first in the mammography exam because the mammography unit is already at a zero-degree position, with the source of x-rays entering the superior portion of the breast and exiting the inferior portion of the breast that rests on the imaging receptor. It must be performed on both breasts.
CC view is ideal for showing if lesions are medial or lateral to the nipple. The CC view also demonstrates if lesions are anterior, or posterior. The CC view best demonstrates medial tissue but on some patients it is limited in the amount of far posterior lateral tissue. The breast should be positioned with two hands to pull the posterior tissue away from the chest wall and avoid folds underneath the breast. The contralateral breast should be brought up on the receptor to reveal the posterior-medial breast tissue, attempts should be made to keep the nipple in profile and centered on the detector, as long as posterior tissue is not sacrificed. The ACR states the nipple should be in profile in at least one view. A potential issue mammographers tend to run into is that the nipple tends to fold under on large breasts, but this can be the natural position on pendulous breasts.
Mediolateral Oblique (MLO) View (in laymen’s terms the side-to-side view)
When the MLO is positioned correctly the pectoralis muscle should be visualized in a shape that is wide superior with an anterior convex border extending down to the level of the nipple. The superior portion of the compression paddle should fall right under the patient’s clavicle, with the front edge of the paddle resting up against the edge of the sternum. Using both hands, the technologist should use the out and up maneuver to get the breast positioned on the detector so that the nipple is in profile and the inframammary fold is visualized open. Ideally, the inframammary fold (IMF) should be visualized without folds which can be accomplished by the mammographer running her fingers down the patient’s abdomen as well as down her back to alleviate folds closest to the detector.
Additional Views
- 90-degree lateral ML/LM – shows benign milk of calcium, helps the radiologist triangulate when a lesion is only seen in one projection and can help demonstrate lesion free of superimposition or magnification. It is especially useful when lesions are medial or lateral.
- Exaggerated CC XCCL/XCCM – shows extreme lateral or medial portions of the breast respectively.
- Cleavage view - shows an extreme medial portion of both breasts.
- Axillary view – shows areas of abnormalities in the axilla area.
- Tangential – not needed as much because of Digital Breast Tomosynthesis (DBT), but in a 2D setting shows calcifications in the skin or it can bring palpable areas into the fatty portion of the breast away from dense breast tissue that superimposes it.
- Rolled views - not needed as much because of Digital Breast Tomosynthesis (DBT), but in a 2D setting can reveals if a lesion seen in only one view is real or simply superimposed breast tissue. It can also help the radiologist know where this lesion is in the opposite view.
- Implant displaced view - shows breast tissue without impedance from a breast implant. It is required only on women who have augmented breast(s). Standard imaging for an augmented breast is four views with implants in place and four views with implant displaced (ID) AKA push backs views.
- Nipple in profile – a dedicated image to demonstrate the nipple in profile when unable to demonstrate a profile view in both of the standard views. It is recommended that this view shows at least two centimeters behind the nipple to reveal the retro areolar tissue without superimposition.
- AC anterior compression – needed sometimes with extra-large breast to show the anterior portion of the breast well separated.
- Spot compression views – Is a dedicated image of one “spot” within the breast. Often used during a diagnostic mammogram to help show borders of lesions without superimposition of tissue.
- Magnification - used mostly to better demonstrate the detail of breast calcifications. Radiologists look for the size, shape, and form of calcifications to help determine if they need to be biopsied or not.
- SIO-superior inferior oblique - an optional additional view used to demonstrate posterior inferior tissue when a standard MLO view cannot.
- LMO – true reverse of the MLO. It is done at about 135 degrees and is used for kyphosis and patients with pacemakers, defibrillators, or port-a-caths.
- From Below (FB) - true reverse of the CC, used for male patients, women with extremely small breast, kyphotic patients and patients with pacemakers, defibrillators, or port-a-caths.
Improve Your Mammography Positioning
The Medical Technology Management Institute (MTMI) has several mammography training courses you can take to improve your imaging practice. If you are a radiologic technologist just starting in the field, our Initial Mammography Training Course will acquaint you with standard positioning practices. The Advanced Mammography Positioning Course takes a more comprehensive approach. Designed for any level mammographer, this hands-on program covers positioning patients with implants, wheelchair patients, kyphotic patients and other special circumstances. Facilities interested in improving their team’s positioning skills and imaging quality can participate in an MTMI individualized consulting program or in-service.
MTMI programs are taught by experts with national reputations in their fields and cover every modality. Our cross-training courses are offered in the classroom and via webinars and prepare you for registry exams, accreditation, and to take your career to the next level. Check out our full catalog of programs, or contact us with questions today!